Migraine and stress
There are strong links between stress and migraine. We explain how managing stress can help if you have migraine.
The link between migraine and stress
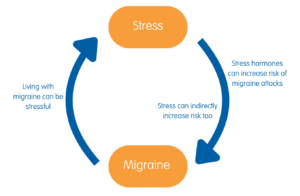
Migraine is not caused by stress. But stress is one of the most commonly-reported migraine attack triggers in people who live with migraine. Living with migraine can itself be stressful. This means it can be easy to end up in a cycle where the more migraine attacks you have, the more stressed you feel. Being stressed then makes you more vulnerable to further attacks.
Lots of different events and situations in your daily life may cause stress. But particular things that people with migraine may find stressful include:
- worrying about when the next attack may happen, or factors that may trigger it, and trying to plan life around it
- catching up on work or activities missed due to migraine attacks
- the impact of migraine on work and finances
- the impact of migraine on caring responsibilities
- how migraine affects social life, relationships and daily life – including pressures to function ‘normally’ and the guilt of cancelling plans, or letting people down
- managing co-morbidities (other health conditions) alongside migraine
- navigating the healthcare system and trying to find treatments that help.
Stress can make the overall impact of living with migraine worse, including your symptoms and the effect it has on your normal day-to-day activities. It can also contribute to the development of chronic migraine – when migraine attacks become much more frequent.
How stress increases risk of migraine attacks
When you are stressed, your body produces a hormone called cortisol. This causes many different changes in your body that may make a migraine attack more likely. This includes how your brain processes pain.
Stress hormones can negatively affect your sleep and your mood too, which can both play a role in migraine. Stress also has an impact on your gut biome – the bacteria and micro-organisms living in your gut. This can make a migraine attack more likely.
There can be lots of ways stress may indirectly increase your risk of a migraine attack too. You might be less likely to stick to regular eating patterns if you’re stressed, for example. Or you might drink more caffeine or alcohol, work longer hours, or stay up later than normal. All of these things may contribute to a migraine attack.
Some people find that if their body has got used to feeling stressed over a long period of time, they get a migraine attack when they stop and relax. This is sometimes called a ‘let-down migraine’. You might notice it happening on a weekend or when you have a break from work. Migraine is often about keeping your body in balance. In this case, a migraine attack happens as the levels of stress hormone in your body decline.
Managing stress with migraine
Managing stress will not stop your migraine altogether. But it may help to reduce the impact of migraine attacks. This includes how many migraine attacks you get, how severe they are and how much they disrupt your life.
It’s impossible to avoid stress entirely. But learning how to manage and cope with it may help. Stress management can involve many things. It might just mean making some simple changes and finding ways to relax. Or it can mean learning techniques aimed at changing the way you think or feel.
Tips for managing stress with migraine
- Pace yourself. When you have migraine, it can be tempting to try and ‘catch up’ on tasks when you have a good day. But this can mean you overdo things, which may leave you more vulnerable to another migraine attack. It’s important to take the time to rest properly while you recover from an attack too. Try to aim for a more balanced, planned approach as much as possible.
- Make time for yourself. Spending time on things you enjoy can be a distraction from ongoing feelings of stress. Try to incorporate small things into your daily life. That might be having a chat with a friend, getting out for a walk, reading a book or spending time on a hobby or interest.
- Be flexible in your plans. It’s good to have small, achievable goals and targets – whether that’s at work or in your personal life. But accept that migraine can change plans. Don’t be afraid to adapt your goals and plans or ask for support when you need to. You do not need to feel guilty about putting your own health first.
- Advocate for your care. Navigating the healthcare system and accessing treatments for migraine can be incredibly stressful. But having the right care and treatment in place can make all the difference to how you feel. We have tips to help you advocate for your care. A friend, partner or family member may be able to support you with this.
- Seek support at work, school or college. The impact on work or education can be one of the most stressful things about living with migraine. We have advice about your rights, tips for managing your migraine, and getting the support you need. Download our toolkits to find out more.
- Know your own migraine. Keeping a headache diary can help you to spot possible triggers and any patterns to your migraine attacks. This may help you to understand your migraine and feel more in control. Bear in mind that it can be easy to mistake early warning signs of an attack for a trigger. If there are no obvious triggers try not spend too much time trying to identify one. It’s very difficult to identify and avoid single triggers, and this can end up causing more stress.
- Plan ahead. If you are worried about future attacks, you may find it helpful to think through what coping strategies you can try in advance. If you are worried about migraine disrupting a particular event, think about what you can do that might lessen the risk. This might mean considering travel times, getting a good night’s sleep beforehand or having snacks and medication on hand.
- Look after yourself. Taking steps to look after your general health can help when it comes to managing stress. This may include getting regular exercise, following a healthy, balanced diet and getting into a good sleep These are all measures known to have a positive impact on migraine too.
- Get support. There are lots of ways you can find support. It can mean talking things over with family or friends, seeking support in the workplace or talking to others in a similar situation. You can also get support from a trained professional, such as a counsellor or therapist. Our helpline offers information and support for everyone affected by migraine.
Mental health charity, Mind have lots more general tips on managing stress. See: mind.org.uk/stress
Relaxation techniques for migraine
Any way that you can find to relax can be helpful if you are feeling stressed. It can be as simple as something you do in your own time that helps you to switch off. Perhaps listening to some music or a podcast, doing something creative, getting outside for a walk or having a warm bath. Exercises like yoga, pilates or even just some gentle stretching can be good for relaxation.
There are also specific techniques you can learn that help with relaxation. The following examples all have some evidence that they can help with migraine.
- Breathing exercises. These include deep breathing and paced breathing exercises. Slowing down your breathing can help to calm your nervous system, making you feel less stressed.
- Progressive muscle relaxation. This is an exercise in which you focus on tensing and relaxing different muscle groups, one at a time. It may help with stress by altering involuntary functions in your body – such as your breathing and heart rate.
- Guided imagery. This is where you focus your attention on a pleasurable or positive image in your mind – such as picturing a calm, safe place.
- Autogenic training. In this technique, you repeat phrases in your mind in order to create feelings of relaxation in your body. These may include warmth and heaviness in your hands and arms, or a slower heartbeat.
It’s better to try and make these exercises a routine part of your daily life that you do if you are feeling stressed. It’s unlikely to be so effective if you only practice these techniques when you feel a migraine attack coming on.
Other behavioural therapies for stress
Behavioural therapies aim to change the way you think or feel. In migraine, they may help you cope better with migraine attacks. They can be particularly helpful when stress is a trigger. In addition to the relaxation techniques discussed above, they include:
- A technique where you learn how to recognise and control involuntary changes in your body. These may happen in response to stress or during a migraine attack.
- Cognitive Behavioural Therapy (CBT). A therapy that can help you change negative thought patterns and behaviours, which can help change how you think and act.
- Mindfulness-based therapies. Mindfulness is a practice where you learn how to pay attention to your actions, feelings and surroundings, in a calm and non-judgemental manner. It can cover a range of different techniques, some tailored to managing stress.
- Acceptance and Commitment Therapy (ACT). A therapy based around the principles of CBT and mindfulness. You learn to move away from unhelpful thoughts by living alongside your migraine, rather than fighting against it.
We have more information about behavioural therapies. Talk to your GP or specialist about how to access to behavioural therapies in your area.
Further information
You may be able to do learn how to do some of the techniques mentioned above yourself, through apps or guides on websites.
- Mind has information on simple relaxation and mindfulness exercises you can do by yourself
- Mind also maintains a library of trusted mental health and wellbeing apps: orchahealth.com
- Young Minds has useful information on helping a child with worry or anxiety
- NHS has self-help guides, tools and activities for mental health, including exercises for stress.
About our information
 This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
Our information has been awarded the PIF TICK quality mark for trustworthy health information.
If you have feedback on our information, please get in touch at: feedback@migrainetrust.org
Last reviewed: February 2026 | Next review due: February 2029
- Sebastianelli G, Atalar AÇ, Cetta I, et al. Insights from triggers and prodromal symptoms on how migraine attacks start: The threshold hypothesis. Cephalalgia. 2024;44(10). doi:10.1177/03331024241287224
- Stubberud A, Buse DC, Kristoffersen ES, et al. Is there a causal relationship between stress and migraine? Current evidence and implications for management. J Headache Pain. 2021;22(1):155. doi:10.1186/s10194-021-01369-6
- Haghdoost F, Togha M. Migraine management: Non-pharmacological points for patients and health care professionals. Open Med (Wars). 2022;17(1):1869-1882. doi:10.1515/med-2022-0598
- Gorenshtein A, Shihada K, Leibovitch L, et al. The association between migraine and gut microbiota: a systematic review. Acta Neurol Belg. 2025;125(4):977-987. doi:10.1007/s13760-025-02779-y
- Sturgeon JA, Ehde DM, Darnall BD, et al. Psychological approaches for migraine management. Anesthesiol Clin. 2023;41(2):341-355. doi:10.1016/j.anclin.2023.02.002
- Hossain MN, Lee J, Choi H, et al. The impact of exercise on depression: how moving makes your brain and body feel better. Phys Act Nutr. 2024;28(2):43-51. doi:10.20463/pan.2024.0015
- Woldeamanuel YW. Exercise patterns and migraine management: a multifaceted approach. Am J Lifestyle Med. Published online June 19, 2025. doi:10.1177/15598276251346394
- Food and mental health. March 2023. mind.org.uk, accessed 13 January 2026
- Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Science. 2015;8(3):143-152. doi:10.1016/j.slsci.2015.09.002
- Mínguez-Olaondo A, Días PA, de Munáin EL, et al. Behavioral therapy in migraine: Expanding the therapeutic arsenal. Eur J Neurol. 2024;31(12):e16414. doi:10.1111/ene.16414


