Stages of a migraine attack
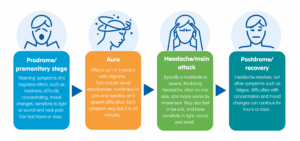
There are well defined stages of migraine attacks, including prodrome, aura, headache and postdrome.
About the stages of migraine attack
If you have migraine, you have recurrent episodes known as migraine attacks. You can get many different symptoms as part of a migraine attack. Some people identify triggers for their migraine attacks. But it can be difficult to know when a migraine attack is going to happen. However, you can often tell the pattern of each attack as they tend to have well-defined stages.
There can be three or four stages of a migraine attack that lead on from each other. Not everyone will experience every stage or find it easy to identify them. The stages can also overlap, with some symptoms continuing across all three or four stages. Each stage can vary in how long and how bad it is. The combination of stages you get may also vary from attack to attack. Overall, a migraine attack may last between four hours and three days, without effective treatment.
Learning to recognise the different stages of a migraine attack can be useful. The different stages can help to tell migraine apart from other types of headache. Recognising these stages can help a doctor with making a diagnosis. Understanding the different stages can also help you to be prepared and know when to take acute medication or adapt your activities.
There are also different self-management strategies you can try if you know a migraine attack is starting, to help you to cope with a migraine attack.
Below, we go through each of the possible stages of a migraine attack in more detail.
Prodrome or premonitory stage
The prodrome stage used to be called the ‘premonitory stage’. It’s also sometimes described as the warning stage, as it helps to warn you that a migraine attack is starting. You may notice certain symptoms in the prodrome stage. These can include:
- feeling very tired (fatigued)
- finding it difficult to think or concentrate
- being more sensitive to light, sound or smell
- neck pain or stiffness
- changes in your mood such as feeling down or irritable
- feeling sick (nausea)
- yawning
- food cravings – especially for sweet foods, such as chocolate
- feeling dizzy
- feeling thirsty
- passing more urine (wee).
You may notice these symptoms hours or sometimes days before the other stages of a migraine attack begin. You may find it helps to predict when an attack is starting.
Aura
Up to a third of people with migraine experience an aura stage as part of their migraine attacks. Not everyone with migraine will have this stage. You may also have a mix of migraine attacks with aura and without aura.
Migraine aura includes a wide range of symptoms that are all related to your nervous system. These symptoms are temporary and may include:
- changes in sight (visual disturbances) such as blind spots, coloured spots or lines and flashing or flickering lights
- numbness or pins and needles
- problems with speech
- hearing loss or changes, such as tinnitus (ringing or buzzing in your ears)
- dizziness or vertigo (sensation of spinning and poor balance).
Less commonly some people may experience muscle weakness. In hemiplegic migraine, you will also have temporary weakness or even paralysis on one side of your body.
Aura is the result of a slow wave of abnormal electrical activity that spreads over the brain during a migraine attack (known as cortical spreading depression). This causes the nerves in your brain to fire in an abnormal way, leading to the symptoms of aura. These changes are temporary and fully reversible. They don’t cause any long-term damage.
Most aura symptoms last from five to 60 minutes. If you have several different aura symptoms, they tend to start one after the other. Aura usually happens before the headache stage. But it can happen at the same time, or even after the headache has started.
It’s also possible to have aura symptoms without any headache at all. This is often referred to as ‘silent migraine’.
Headache or main attack stage
This stage involves headache, which is usually moderate or severe in intensity. The headache in migraine is often described as a throbbing pain, and is made worse by movement. It’s often on one side of the head, especially at the start of an attack. However, you can get pain on both sides, or all over the head.
The headache may be associated with feeling sick (nausea) or being sick (vomiting), and you may feel more sensitive to light, sound and smell. Painkillers work best if you take them as soon as the headache stage starts.
For most people, a migraine headache will slowly fade away over the course of several hours. But some people find their headache stops more rapidly. Sleep seems to help many people, with even just an hour or two sometimes enough to end an attack. This can be particularly helpful in children.
Postdrome or recovery stage
This is the final stage of a migraine attack. After the headache and other symptoms have resolved, you may feel drained, fatigued or even ‘hungover’ for some time. It can take hours or days for these feelings to disappear. Symptoms can be similar to those of the first (prodrome) stage. Fatigue, difficulty concentrating and mood changes are common symptoms. You may continue getting symptoms such as sensitivity to light and sound in this phase too.
With many migraine symptoms continuing right into this postdrome stage, it’s important to take the time you need to fully recover.
About our information
 This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
Our information has been awarded the PIF TICK quality mark for trustworthy health information.
If you have feedback on our information, please get in touch at: feedback@migrainetrust.org
Last reviewed: October 2025 | Next review due: October 2028
- NICE Clinical Knowledge Summaries. Migraine. August 2025. cks.nice.org.uk, accessed 22 September 2025
- British Association for the Study of Headache (BASH). National Headache Management System for Adults. 2019. bash.org.uk
- StatPearls Publishing. Migraine headache. 5 July 2024. ncbi.nlm.nih.gov/books, accessed 23 September 2025
- Thuraiaiyah J, Christensen RH, Al-Khazali HM, et al. Overlap between perceived triggers, premonitory symptoms and symptom persistence across migraine phases: A REFORM study. Cephalalgia. 2025;45(8). doi:10.1177/03331024251364234
- International Headache Society. IHS classification ICHD-3. ichd-3.org, accessed 22 September 2025
- Schwedt TJ, Lipton RB, Goadsby PJ, et al. Characterizing prodrome (premonitory phase) in migraine. Neurol Clin Pract. 2025;15(1). doi:10.1212/CPJ.0000000000200359
- Lisicki M, Schoenen J. Old habits die hard: dietary habits of migraine patients challenge our understanding of dietary triggers. Front Neurol. 2021;12. doi:10.3389/fneur.2021.748419
- Thomsen AV, Ashina H, Al-Khazali HM, et al. Clinical features of migraine with aura: a REFORM study. J Headache Pain. 2024;25(1):22. doi:10.1186/s10194-024-01718-1
- StatPearls Publishing. Migraine with aura. 29 February 2024. ncbi.nlm.nih.gov/books, accessed 24 October 2025
- Dodick DW. A phase‐by‐phase review of migraine pathophysiology. Headache: The Journal of Head and Face Pain. 2018;58(S1):4-16. doi:10.1111/head.13300
- Blau JN. Resolution of migraine attacks: sleep and the recovery phase. J Neurol Neurosurg Psychiatry. 1982;45(3):223-226. doi:10.1136/jnnp.45.3.223
- Christensen RH, Eigenbrodt AK, Ashina H, et al. What proportion of people with migraine report postdromal symptoms? A systematic review and meta-analysis of observational studies. Cephalalgia. 2023;43(10). doi:10.1177/03331024231206376


