Migraine attack triggers
There are many factors that may trigger migraine attacks. We look at some of the most common migraine triggers here.
About migraine triggers
A migraine trigger is something that seems to cause or worsen a migraine attack. If you have migraine, you may be keen to try and identify your triggers as a way to help manage your migraine. But this isn’t always easy. Many people don’t have any obvious triggers, and some – such as weather changes – can’t be controlled.
Although trying to avoid known triggers can be helpful for some people, focusing on this too much can cause more harm than good. We have more information on identifying and managing triggers at the end of the page.
Migraine threshold theory
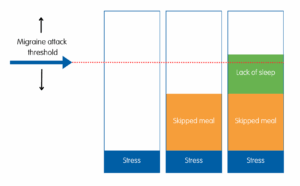
When you live with migraine, it can feel like almost anything might trigger an attack. In reality, only a few factors make a significant difference to your risk of getting an attack on their own. It’s more likely to be a combination of several things that leads to a migraine attack. For example, you may find that you are more likely to have migraine attacks when you:
- have not eaten or skipped meals
- have not had much sleep
- are under a lot of stress.
While one of these things on its own may be less likely to lead to a migraine attack, two or three together may push you over the threshold for an attack.
This is known as the ‘threshold theory’. A threshold is a level when something starts to happen – like a migraine attack. Your threshold may shift up or down, making you more or less sensitive to an attack at different times. This can be influenced by things like hormonal changes and illness.
Migraine triggers and warning signs
Sometimes, what you think is a migraine trigger may actually be an early symptom of a migraine attack. This is known as the ‘prodrome’ or ‘warning’ stage of a migraine attack.
During this stage, you may get symptoms such as mood changes, neck stiffness or pain, and cravings for certain foods. You may also notice you’re more sensitive to light, sound or smells.
It can be easy to mistake these warning signs for triggers. For example:
- if you eat chocolate to satisfy a craving in the prodrome stage, you may think that chocolate is a trigger
- if you are more sensitive to light in the warning stage, you might think bright lights are a trigger
- if you have neck pain or stiffness as a prodrome symptom, you might think this is a trigger.
If you believe something to be a trigger when it’s not, you might try to avoid it for no reason. But if you know that something is a warning sign, it could help you to spot an attack early and get the treatment you need sooner. This may reduce how much impact the migraine attack has.
It’s not easy to tell whether something is a warning sign or a trigger. But keeping a diary may help. We have more information on this below.
Common migraine triggers
Below we list some of the most commonly-reported migraine triggers. It’s important to bear in mind that triggers can be different for everyone. You may not have any of the triggers listed here, or you may have identified different triggers to those listed.
Many people find it’s a change in their usual routine that triggers a migraine attack. This relates to many of the factors below, including sleep patterns, mealtimes, caffeine and stress.
Migraine is frequently linked to change in hormone levels, particularly oestrogen. If you have periods, you may find you are more likely to have migraine attacks around the start of your period. This is known as menstrual migraine. Rapid changes in your hormone levels can also trigger migraine attacks in the lead up to menopause. But after menopause, migraine attacks may become less severe and less frequent.
Stress is one of the most commonly-reported triggers for migraine attacks. This is thought to be down to a hormone that you produce when you’re stressed, which may make migraine attacks more likely. Some people find that their migraine attacks start when they stop feeling stressed, and stress hormones decline. They may find that they are more likely to have migraine attacks at a weekend or on holiday, when they come to relax. This is sometimes called a ‘let-down migraine’.
Many people report lack of sleep as a migraine attack trigger. Sleep deprivation may have a direct effect on the migraine pathway in the brain. Some people find that having more sleep than usual, for example having a lie-in on a weekend, can increase the risk of a migraine attack. A change in your usual sleep patterns can have the same effect. Good sleep hygiene, including keeping to regular bedtimes and wake times, may help.
Fasting (not eating) or missing meals causes a drop in your blood sugar levels. Many people find migraine attacks can become more frequent and more severe after a period without eating. Making sure you stick to regular mealtimes and not going too long between meals may help. We have more information on healthy eating for migraine on our Migraine and diet page.
Having too much caffeine can lead to a migraine attack for some people. However, cutting out caffeine suddenly can also trigger migraine attacks. If you think caffeine may be a trigger, it’s best to try and gradually cut down the amount you have, rather than stopping suddenly. Caffeine is in tea, coffee and cola, as well as chocolate and some over-the-counter painkillers.
Many people find alcohol to be a migraine trigger. Red wine is the most common alcoholic drink reported as trigger. If alcohol does affect you this way, it may not happen every time you drink. It can depend on how much you have drunk, and what other factors may be present – such as if you are tired or stressed.
Many people with migraine identify certain foods as migraine attack triggers. Common examples include chocolate, dairy, and foods containing tyramine, monosodium glutamate (MSG) and nitrates. However, there is a lack of evidence to support food triggers for migraine. Studies looking into this have had inconsistent results.
Also, some foods, such as chocolate, are often mistaken as a trigger, when craving these foods may actually be a symptom of the prodrome phase. Because of this, it’s not recommended to try cutting out different foods unless you are sure a specific food triggers your migraine. You can find out more about possible food triggers for migraine in our information on migraine and diet.
Not drinking enough fluids can lead to dehydration. This can appear to trigger or worsen migraine attacks for some people. It’s usually enough to aim for six to eight cups or glasses of fluid a day to keep hydrated.
Many people with migraine seem to be sensitive to changes in the weather. You may find that changes in temperature, barometric pressure and humidity can make you more likely to have a migraine attack.
Bright or flickering lights, noise and odours are all frequently reported as triggers for migraine attacks. You may also find they make migraine attacks worse. Both sunlight and artificial lighting can be a problem for people with migraine. However, many people become more sensitive to light, noise and odours during a migraine attack. This can make it difficult to know whether these things are triggers, or early symptoms of a migraine attack.
Looking at screens for a long time has been linked to increased risk of migraine attack for some people. This may be due to the light emitted by computer screens. Eye strain from too much screen use can also lead to more tension-type headaches. It’s important to take regular breaks from the screen. It might also help if you use an anti-glare or anti-blue light screen or filter, or adjust the brightness of your screen. Good lighting may also help.
Intensive exercise appears to trigger attacks for some people with migraine. However there is limited evidence about this. It might be more likely if you are not normally very active. For most people, doing regular exercise if you are able to, and at a level you find manageable can be a positive thing. Exercise can be helpful in preventing migraine attacks. This is because it stimulates the body to release natural painkillers. It’s also good for general health, which means you may be more able to cope with migraine attacks.
Identifying and managing triggers
Keeping a migraine diary may help you to notice any patterns with your migraine attacks. You can record things like:
- the times you wake up and go to sleep
- your mealtimes and what you have had to eat
- how much caffeine or alcohol you drink
- your mood and stress levels
- the weather
- your menstrual cycle, if you have one
- where you have been that day and possible triggers (such as lighting or noise).
In some cases, you may be able to identify potential triggers that are relatively easy to manage. Keeping a diary may also show that some things you believed to be triggers do not have as much impact as you thought. A migraine diary can also help you to be more alert to your warning signs.
Regular routine
It often seems to be a change in someone’s usual routine that triggers a migraine attack. This can include a change in sleep routine, eating at different times, drinking more or less caffeine or even relaxing after a period of stress. Aiming to keep to a regular routine as much as possible can be helpful.
Sometimes a change in routine is unavoidable. For example you may be travelling for work or going away on holiday. It can help to be prepared for these situations. You might think about taking snacks on long journeys for example, so you don’t go too long without eating. Make sure you have migraine medication on hand so if you do feel an attack starting, you can treat it quickly.
Avoiding triggers
Avoiding individual triggers can be extremely difficult, especially when it involves changing your lifestyle or routines. It can be particularly hard when migraine attacks tend to be triggered by a combination of things. Many of these factors can be things outside of your control, like the weather or changes in hormones. Also, something you have identified as a trigger may not cause a migraine attack every time.
Trying to identify and avoid individual triggers can take a lot of time and effort. This can make you feel anxious and have a negative impact on other parts of your life.
It’s also important to be realistic about what impact identifying and avoiding triggers will have. If you are able to avoid your triggers, you may be able to reduce how often you have migraine attacks, but you may not stop having them altogether. Many people also need treatment to control their condition.
Lifestyle adjustments
It can be more worthwhile to focus on general adjustments to your lifestyle that may help. This may include:
- being more active or getting regular exercise if you are able to, at a level you find manageable
- aiming for a healthy, balanced diet
- trying positive ways to manage stress
- taking steps to improve sleep routine.
These things may potentially have a positive impact on your migraine. Making adjustments to lifestyle where you can may also help with your general health. This can mean you feel more able to cope with migraine attacks. Talk to your GP if you need guidance on lifestyle changes you can make.
About our information
 This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
This information has been written by The Migraine Trust Information and Support Services team. It has been reviewed by our panel of expert health professionals and people affected by migraine.
Our information has been awarded the PIF TICK quality mark for trustworthy health information.
If you have feedback on our information, please get in touch at: feedback@migrainetrust.org
Last reviewed: September 2025 | Next review due: September 2028
- Marmura MJ. Triggers, protectors, and predictors in episodic migraine. Curr Pain Headache Rep. 2018;22(12):81. doi:10.1007/s11916-018-0734-0
- Sebastianelli G, Atalar AÇ, Cetta I, et al. Insights from triggers and prodromal symptoms on how migraine attacks start: The threshold hypothesis. Cephalalgia. 2024;44(10). doi:10.1177/03331024241287224
- NICE Clinical Knowledge Summaries. Menopause. November 2024. cks.nice.org.uk, accessed 11 February 2025
- Casanova A, Vives‐Mestres M, Donoghue S, et al. An observational study of self‐reported migraine triggers and prospective evaluation of the relationships with occurrence of attacks enabled by a smartphone application (App). Headache: The Journal of Head and Face Pain. 2022;62(10):1406-1415. doi:10.1111/head.14328
- Thuraiaiyah J, Christensen RH, Al-Khazali HM, et al. Overlap between perceived triggers, premonitory symptoms and symptom persistence across migraine phases: A REFORM study. Cephalalgia. 2025;45(8). doi:10.1177/03331024251364234
- International Headache Society. The International Classification of Headache Disorders, 3rd edition (ICHD-3). ichd-3.org, accessed 30 July 2025
- Kim S, Park JW. Migraines in Women: A focus on reproductive events and hormonal milestones. Headache and Pain Research. 2024;25(1):3-15. doi:10.62087/hpr.2024.0003
- Ornello R, De Matteis E, Di Felice C, et al. Acute and preventive management of migraine during menstruation and menopause. J Clin Med. 2021;10(11). doi:10.3390/jcm10112263
- Pavlović JM. The impact of midlife on migraine in women: summary of current views. Womens Midlife Health. 2020;6:11. doi:10.1186/s40695-020-00059-8
- Iliopoulos P, Damigos D, Kerezoudi E, et al. Trigger factors in primary headaches subtypes: a cross-sectional study from a tertiary centre in Greece. BMC Res Notes. 2015;8:393. doi:10.1186/s13104-015-1390-7
- Hindiyeh NA, Zhang N, Farrar M, et al. The role of diet and nutrition in migraine triggers and treatment: a systematic literature review. Headache: The Journal of Head and Face Pain. 2020;60(7):1300-1316. doi:10.1111/head.13836
- Tu YH, Chang CM, Yang CC, et al. Dietary patterns and migraine: insights and impact. Nutrients. 2025;17(4):669. doi:10.3390/nu17040669
- Arca KN, Halker Singh RB. Dehydration and Headache. Curr Pain Headache Rep. 2021;25(8):56. doi:10.1007/s11916-021-00966-z
- Water, drinks and hydration. May 2023. nhs.uk, accessed 1 August 2025
- Roy S, Iktidar MA, Chowdhury S, et al. Increased screen time and its association to migraine and tension-type headache: a cross-sectional investigation among Bangladeshi students. BMJ Neurol Open. 2024;6(1):e000656. doi:10.1136/bmjno-2024-000656
- Abou Hashish EA, Baatiah NY, Bashaweeh AH, et al. The online learning experience and reported headaches associated with screen exposure time among Saudi health sciences students during the COVID-19 pandemic. BMC Med Educ. 2022;22(1):226. doi:10.1186/s12909-022-03235-8
- Kaur K, Gurnani B, Nayak S, et al. Digital eye strain – a comprehensive review. Ophthalmol Ther. 2022;11(5):1655-1680. doi:10.1007/s40123-022-00540-9
- Varkey E, Cider Å, Carlsson J, et al. Exercise as migraine prophylaxis: A randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31(14):1428-1438. doi:10.1177/0333102411419681
- NICE Clinical Knowledge Summaries. Migraine. August 2024. cks.nice.org.uk, accessed 1 August 2025


